Abstract
Methemoglobinemia is a rare overlooked differential diagnosis in patients with cyanosis and dyspnea unrelated to cardiopulmonary causes.
Methemoglobin results from oxidation of ferrous iron to ferric iron within the heme moiety of hemoglobin . In healthy individuals, less than 1% of hemoglobin is present in the oxidized form (methemoglobin), which has limited ability to carry oxygen, however with increased oxygen affinity at the remaining binding sites .This results in decrease of oxygen delivery to tissue leading to hypoxaemia and lactic acidosis.
Methemoglobin reductase enzyme deficiency is either type I or type II; type I: Cytochrome b5 reductase deficiency, demonstrable only in the erythrocytes, presents as uncomplicated, benign methemoglobinemia, and associated with a normal life expectancy with only fatigue and dyspnea being the most commonly reported symptoms.
Hereditary type II methemoglobinemia, is global (affects both red and white blood cells) and is associated with severe neurologic dysfunction and reduced life expectancy . The enzyme's activity is less than 20% of normal.
Type II congenital methemoglobinemia constitutes approximately 10% of all cases of congenital methemoglobinemia and usually causes death within the first few years of life
There is a significant delay in the onset of symptoms in a patient with type I hereditary methemoglobinemia, as most studies indicate that patients are asymptomatic in infancy and childhood.
we report a 29 year old Indian non-smoker male, his story started 6 months prior to presentation when he had generalized fatigue and discoloration of hands. He presented with persistent polycythaemia with elevated hemoglobin level. The patient was misdiagnosed in another center as polycythaemia and treated with Imatinib. The diagnosis of PV was revisited and ruled out in view of negative JAK2, normal erythropoietin level and absence of features of panmyelosis.
Clinical cyanosis and low oxygen saturation in the presence of normal arterial oxygen tension was highly suggestive of methemoglobinemia.
Arterial blood gas (ABG) revealed a methemoglobin level of 38% (normal: 0-1.5%). Cytochrome B5 reductase (Methemoglobin reductase B) wasdeficient at level of <2.6 U/g Hb) (normal: 6.6-13.3), consistent with methemoglobin reductase (cytochrome b5) deficiency and hence the diagnosis of congenital methemoglobinemia was established.
The role of Imatinib in provoking methemoglobinemia is questionable and association between Imatinib and methemoglobinemia never described before. There was no history of other drugs offended in aggravating the patients' symptoms and cyanosis.
The patient started on Vitamin C 500 mg for which he responded well with less cyanosis and significant reduction of methemoglobin level.
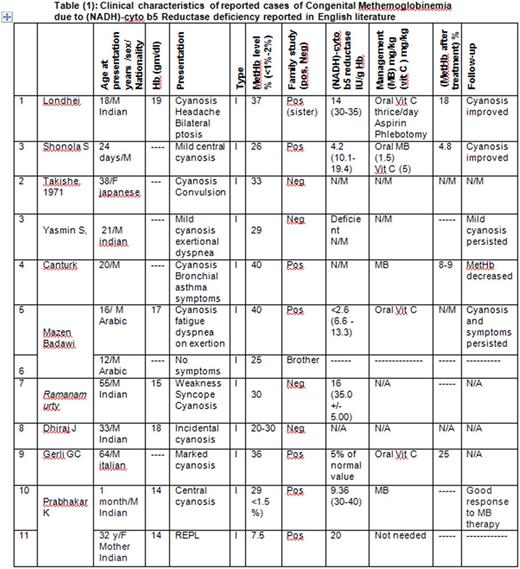
Upon extensive review of English literature for cases of congenital Methaemoglobinaemia due to deficiency of cytochrome b5 reductase, we found 23 cases diagnosed as type I (including the case reported here).
17 cases (~74%) of type I and 6 cases (27%) of type II. There is male predominance (73%) versus 26% in females. Almost half of reported cases (12 cases; 52%) are indian, 2 Japanese, 3 English, 2 Arabic, one Spanish and one Italian.
For type I, the median calculated age is 31 years with cyanosis and shortness of breath being the most common sign and symptom.
For type II: Six cases were reported, all in pediatric age group with median calculated age at presentation is 6 years with neurologic manifestations and mental retardation are the most common type II associated symptoms.
Congenital methemogobinemia is a rare underreported hemoglobin disease. Due to lack of systematic epidemiological studies it is usually under investigated and frequently clinically missed especially when presenting in adulthood.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.